Medicare & Medicaid
Roughly 477,000 jobs could be lost in healthcare, including in hospitals, doctors' offices, clinics, pharmacies and nursing homes.
Hospitals that are already struggling will lose funding, say the Democratic state treasurers of Republican-proposed cuts.
The 14 to 13 vote was along party lines.
That would constitute 34% to 39% of expansion enrollees ages 19 to 55, the data shows.
MA plans have faced recent headwinds of declining payment rates, medical cost pressures, regulatory burden and less favorable star ratings.
Transaction is estimated to be worth about $3.7 billion.
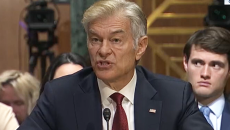
Trump's nominee to head CMS indicated he intended to go after upcoding practices in the Medicare Advantage program.
CMS projects $750 million in savings from ending the four models early, but stopped short of saying where the savings would occur.
Hospitals would face the largest revenue losses and burden of uncompensated care increases, report finds.
More practices will close and Medicare patients will pay the price, says AMA President Dr. Bruce A. Scott.